Menopause is a natural biological transition marking the permanent cessation of menstrual periods and the end of a woman's reproductive years. This transition is characterised by significant hormonal changes, particularly a decline in estrogen levels, which can profoundly affect various aspects of health, including bone health. Understanding these hormonal shifts and their implications is crucial for managing menopause symptoms and preventing long-term health issues.
Most women experience menopause between the ages of 45 and 55, making it a critical health milestone to watch for either in your journey or that of your mother. During menopause, women's musculoskeletal health is significantly affected due to declining estrogen levels. This leads to symptoms such as joint pain, loss of muscle mass, and decreased bone density, increasing the risk of osteoporosis and fractures. Additionally, fat distribution and metabolism changes can further impact MSK health, affecting overall mobility and quality of life.
Understanding the Human Body and Hormones
Before diving into the specifics of menopause, it's essential to grasp the basics of how hormones function in the body. Hormones are chemical messengers produced by glands in the endocrine system that regulate various bodily functions, including growth, metabolism, and reproductive processes. In women, the ovaries produce several key hormones, including estrogen and progesterone, which play critical roles in the menstrual cycle and overall health.
The ovaries produce two key hormones — estrogen and progesterone. Estrogen supports female development, bone and vaginal health, while progesterone prepares the uterus for pregnancy by thickening the uterine lining. Together, they regulate the menstrual cycle and maintain reproductive health.
Key Hormonal Changes During Menopause
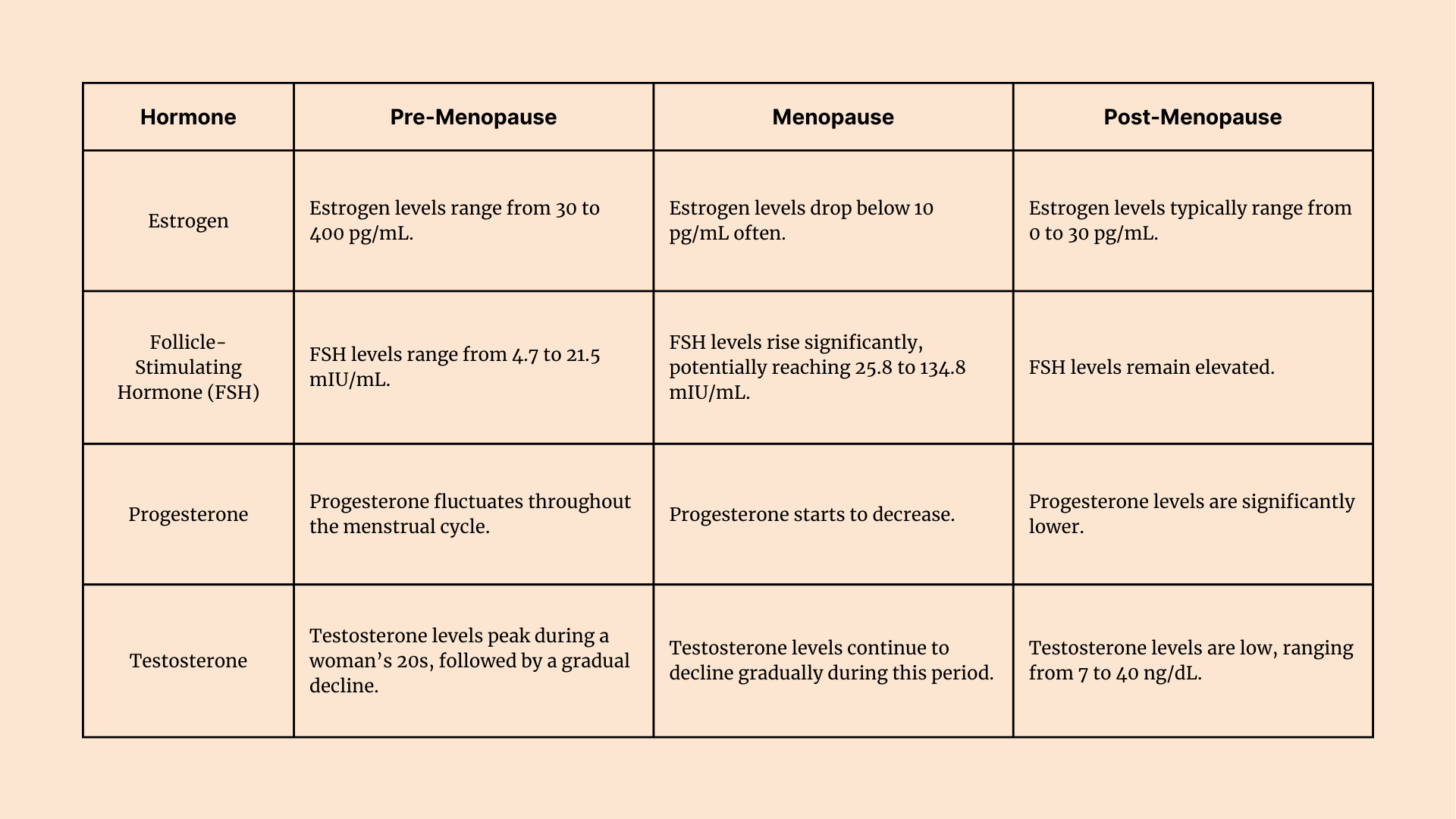
- Estrogen
Estrogen is essential for regulating the menstrual cycle and supporting various systems in the body, including the cardiovascular, skeletal, and reproductive systems. Regarding musculoskeletal (MSK) health, estrogen plays a vital role in maintaining bone density, muscle mass, and joint health. It helps balance bone formation and resorption by regulating osteoblasts (bone-building cells) and osteoclasts (bone-breaking cells).
During menopause, estrogen levels drop significantly, disrupting this balance and leading to weakened bones, muscle loss, and increased MSK pain — contributing to conditions like osteoporosis and osteoarthritis.
- Progesterone
Progesterone is primarily known for preparing the uterus for pregnancy and supporting early gestation. Beyond reproduction, it also contributes to bone formation by stimulating the activity of osteoblasts.
During menopause, progesterone levels decline alongside estrogen. Though its MSK role is less defined, this reduction can diminish osteoblast activity, contributing to slower bone formation and further bone density loss.
- Testosterone
Testosterone, though produced in smaller amounts in women, supports libido, mood stability, and energy levels. MSK health contributes to maintaining muscle strength and bone density.
During menopause, testosterone levels may also decline, potentially reducing muscle mass and affecting overall physical strength. Emerging research suggests it may play a supportive role in preserving bone health in postmenopausal women.
The Role of Estrogen in Bone Health
Estrogen helps preserve bone density by suppressing osteoclast activity (which breaks down bone) and promoting osteoblast function (which builds new bone). This balance ensures that bones stay strong and regenerate at a healthy rate.
During menopause, a sequence of changes in bone health unfolds due to declining estrogen levels:
- Bone Resorption Increases: Lower estrogen levels cause osteoclasts to become overactive, breaking down bone tissue faster than it can be rebuilt.
- Bone Density Declines Sharply: As bone breakdown outpaces bone formation, women can lose up to 10% of their bone density within the first five years after menopause.
- Osteopenia and Osteoporosis Develop: Reduced bone density leads to osteopenia (low bone mass), which, if left unmanaged, can progress to osteoporosis — a condition marked by fragile, fracture-prone bones.
Other Hormonal Factors Affecting Bone Health
In addition to estrogen, other hormones influence bone health during menopause:
- Progesterone: Supports osteoblast activity but declines during menopause, reducing new bone formation.
- Parathyroid Hormone (PTH): Regulates calcium levels; imbalances can worsen bone loss.
- Vitamin D & Calcitonin: Essential for calcium absorption and deposition in bones; deficiencies exacerbate osteoporosis risks.
- Cortisol (Stress Hormone): Chronic stress elevates cortisol levels, which can accelerate bone resorption.
Menopause: What It Is and How It Affects Hormones
Menopause is defined as the point when a woman has not had a menstrual period for 12 consecutive months. This transition is typically experienced between the ages of 45 and 55, with the average age around 51. It is preceded by a phase known as perimenopause, which can begin several years earlier and is marked by increasingly irregular periods and hormonal fluctuations. The primary hormonal change during menopause is a sharp decline in estrogen production by the ovaries. Estrogen is crucial in maintaining bone density, regulating menstrual cycles, and supporting other bodily functions.
Menopause Symptoms:
Menopause symptoms can vary widely among women but commonly include:
- Hot Flashes: Sudden feelings of heat, often accompanied by sweating and flushing.
- Night Sweats: Hot flashes that occur at night, disrupting sleep.
- Vaginal Dryness: Decreased moisture in the vagina, leading to discomfort during sex.
- Mood Changes: Emotional changes, such as irritability or depression.
- Sleep Disturbances: Difficulty sleeping or insomnia.
Perimenopause Symptoms:
Perimenopause, the transition period leading up to menopause, can last several years and is marked by irregular menstrual cycles and increased variability in hormone levels. Symptoms during this phase may include:
- Irregular Periods: Changes in menstrual cycle length and frequency.
- Mood Changes: Similar to menopause, mood swings and irritability are common.
- Hot Flashes: These can begin during perimenopause and continue into menopause.
Hormonal Changes and Bone Health
The decline in estrogen levels during menopause significantly impacts bone health. Estrogen helps maintain bone density by regulating the activity of osteoclasts (cells that break down bone) and osteoblasts (cells that build bone). When estrogen levels drop, bone resorption begins to outpace bone formation, leading to a decline in bone density and a heightened risk of osteoporosis.
While menopause and hormonal changes are widely discussed, far less attention is given to how menopause specifically impacts musculoskeletal (MSK) health. This is a critical gap in awareness. Here, we bring you key insights from recent scientific research on the lesser-known but deeply important relationship between menopause and MSK health.
Why this focus? Because MSK health deteriorates significantly around menopause, with real consequences for mobility, agility, recovery, and injury risk. Understanding this connection is essential to protecting long-term physical function and quality of life.
Osteoporosis
Osteoporosis is a condition characterised by weakened bones more susceptible to fractures. It is a significant concern for postmenopausal women due to the loss of estrogen's protective effects on bone health. Common sites for osteoporotic fractures include the spine, hips, and wrists.
Impact of Hormonal Changes on Musculoskeletal Health
The musculoskeletal system, which includes bones, muscles, and joints, is significantly affected by the hormonal changes of menopause. The loss of bone density not only increases the risk of fractures but also contributes to changes in posture and mobility. For example, vertebral fractures can lead to a hunchback posture (kyphosis.)
Rate of Bone Loss: Perimenopause vs. Postmenopause
The rate of bone loss differs between perimenopause and postmenopause. During late perimenopause, bone loss accelerates due to fluctuating estrogen levels, with annual losses in the lumbar spine often exceeding 2%. In contrast, postmenopause sees a continued but slightly slower rate of bone loss, typically around 1.3-1.5% annually. The first few years after menopause are critical, with significant bone density loss occurring during this period.
Factors Contributing to Accelerated Bone Loss in Late Perimenopause
Several factors contribute to the accelerated bone loss observed in late perimenopause:
- Hormonal Fluctuations: The variability in estrogen levels disrupts the bone formation and resorption balance.
- FSH Levels: Follicle-stimulating hormone (FSH) is a hormone released by the brain (specifically, the pituitary gland) that helps regulate the menstrual cycle and supports reproductive function by prompting the ovaries to produce estrogen and mature eggs.
During menopause, as the ovaries produce fewer eggs and less estrogen, FSH levels rise sharply in an attempt to stimulate hormone production. This hormonal imbalance creates a feedback loop that signals the body to produce even more FSH. Higher FSH levels have been linked to increased bone resorption, contributing to bone loss during the menopausal transition.
- Lifestyle Factors: Inadequate diet (low calcium and vitamin D), lack of exercise, smoking, and excessive alcohol consumption can exacerbate bone loss.
Managing Hormonal Imbalance and Bone Health
While hormonal changes during menopause are inevitable, there are strategies to manage symptoms and protect bone health:
Lifestyle Changes:
- Diet: Ensure adequate intake of calcium and vitamin D.
- Exercise: Engage in weight-bearing exercises to maintain bone density.
- Limit Alcohol Consumption: Excessive alcohol disrupts calcium absorption and hormone levels, weakening bones and increasing fracture risk. Its impact on bone health is often more significant than smoking — especially around menopause.
Medical Interventions:
- Hormone Replacement Therapy (HRT): This can help alleviate symptoms and protect bone health, though it should be used under medical supervision due to potential risks.
- Non-Hormonal Medications: Options like bisphosphonates can help prevent bone loss.
Monitoring Bone Health:
Regular bone density tests can help identify early signs of osteoporosis and guide treatment decisions.
Early Menopause Symptoms and Risks
Early menopause, occurring before age 45, can increase the risk of osteoporosis due to a more extended period without the protective effects of estrogen. Women experiencing early menopause should be particularly vigilant about maintaining bone health through lifestyle adjustments and medical interventions.
Conclusion
Menopause marks a significant phase in a woman's life, characterised by profound hormonal changes that can impact various aspects of health, particularly bone health. Understanding these changes and taking proactive steps to manage symptoms and protect bone density are crucial for maintaining quality of life during and after menopause. By combining lifestyle modifications with medical interventions when necessary, women can mitigate the risks associated with hormonal imbalances and ensure a healthier transition through this life stage.











